Recently, the federal government unveiled the first in a series of new rules designed to protect patients from financial hardship due to surprise medical bills and balanced billing. Surprise billing typically occurs when you receive emergency care from an out-of-network provider or when you receive nonemergency care at an in-network facility but are inadvertently (and often unknowingly) treated by an out-of-network health care provider.
The new protections apply to most emergency services, air ambulance services from out-of-network providers and nonemergency care from out-of-network providers at certain in-network facilities, including in-network hospitals and ambulatory surgical centers.
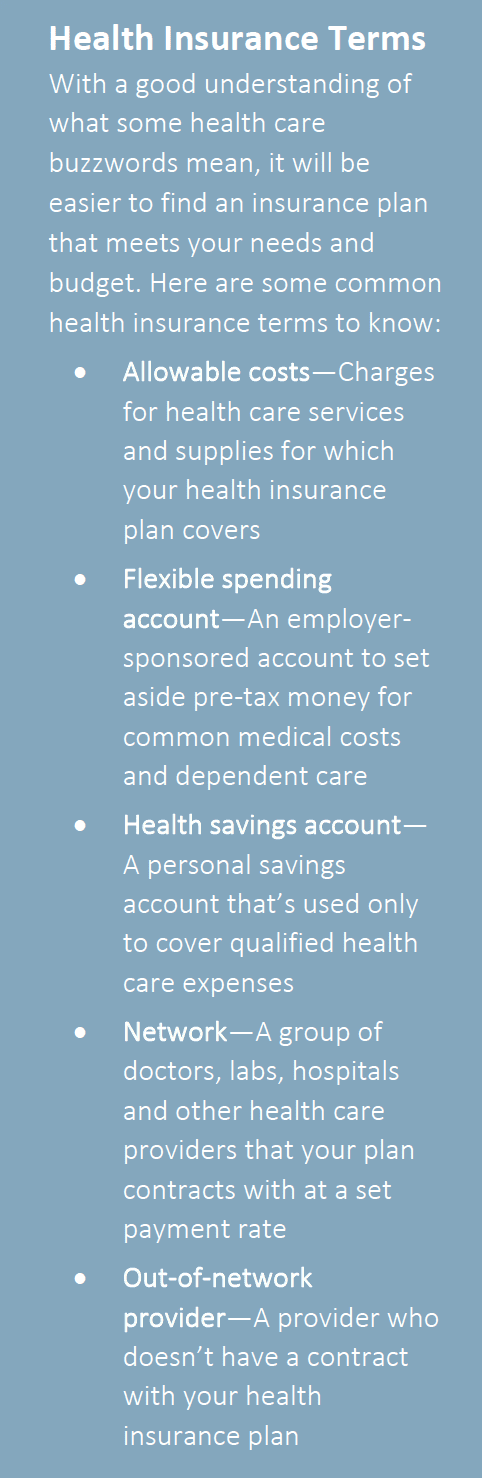
The rule will restrict excessive out-of-pocket costs to consumers from out-of- network and balance billing. This practice is already banned by Medicare and Medicaid. The interim rule extends protection to people insured through employer-sponsored and commercial health plans as well.
The interim final rule will take effect on Jan. 1, 2022.
The Importance of Shopping Around for Health Care
As you look to take control of your health care and spending habits, you should get acquainted with the concept of shopping around for health care services. This can be accomplished by making cost comparisons, understanding differences in quality of service and using a personal cost-benefit equation to determine when the expense is worthwhile.
You can save money by asking questions and searching for the most economical option that doesn’t sacrifice value. For example, consider the following actions:
- Ask about costs for treatments and
- Ask about alternative
- Request generic drugs instead of a brand
- Call around to find the lowest cost procedures, treatments and
- Search online resources for quality and price